Background
Waldenström's Macroglobulinemia (WM) is an incurable B-cell neoplasm characterized by serum monoclonal immunoglobulin M (IgM) and clonal lymphoplasmacytic cells infiltrating the bone marrow (BM). Smoldering WM (sWM) is the asymptomatic/indolent form with a high risk of progressing to symptomatic WM requiring treatment whereas IgM monoclonal gammopathy of undetermined significance (IgM MGUS) is an early precursor stage of WM. Despite recurrent and activating mutations, including MYD88, CXCR4, ARID1A, KMT2D, and CD79B have been identified, the genetic basis for WM and the risk of progression of IgM MGUS to WM remain to be fully elucidated.
Methods
Based on the mutational profiling of WM and our previous wide transcriptome analyses on BM CD19+ and CD138+ cells of patients with WM and IgM MGUS, we decided to investigate the mutation status of these patients as follows: WM (n=10), sWM (n=7), and IgM MGUS (n=5), by performing high throughput targeted AmpliSeq next generation sequencing on 117 target genes potentially involved in B-cell lymphomagenesis and in the risk of progression of IgM MGUS to WM (Trojani A. et al. Cancers, 2021).
Results
We identified genetic aberrations in multiple genes, including previously described classic mutations in MYD88 (L260P alias L265P) found in 82.3% (14/17) of WM/sWM patients and in 60% (3/5) of IgM MGUS subjects. The CXCR4 mutation (S338Ter) was detected in 23.5% of CD19+ cells of WM patients, whereas it was absent in IgM MGUS subjects.
Interestingly, we also identified new mutated genes, including WNK2 somatic mutations affecting 47% of WM patients, for which a recurrent allelic variant (V1635Ter) was observed, and BCL9 with a recurrent frameshift variant (P516Lfs) identified in 29.4% of WM patients exclusively in the CD19 cell fraction. The BCL9 (P516Lfs) variant was also detected in the B cells of one IgM MGUS patient.
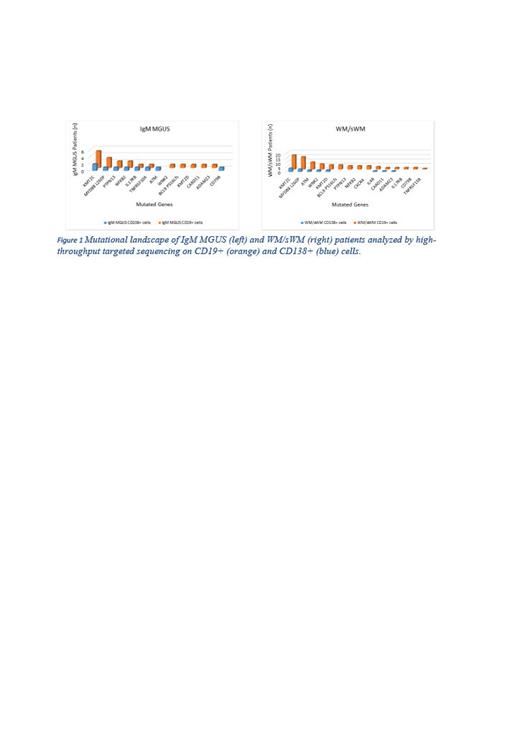
Moreover, sequencing evaluation revealed recurrently frameshift or missense mutations involving NFKB2 (L473Afs), PTPN13 (P1546Tfs), CARD11 (S622del), KMT2C (I823T), and ATM in WM and IgM MGUS patients (Figure 1). Of interest, KMT2C (also known as MLL3) exhibited a somatic hypermutated phenotype in both CD19+ and CD138+ cells of WM and IgM MGUS samples. The KMT2C mutations were not mutually exclusive with those involving KMT2D in our cohort of patients.
Conclusion
The present genomic analysis revealed new insights into the mutational landscape of Waldenström Macroglobulinemia, providing evidence of the recurrence of some variants in subjects with IgM MGUS as well. Notably, we uncovered new genetic mutations with somatic variants recurrently observed (n≥3) in KMT2C, WNK2, BCL9, PTPN13, CARD11 and NFKB2 genes.
These recurring somatic events provide a genomic basis for future research and a better understanding of the WM pathogenesis as well as the risk of transformation of IgM MGUS to WM.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal